Where does CAR T-cell cancer therapy stand after its FDA approval?
After being approved by the FDA, CAR T-cell cancer therapy progresses in its treatment of pediatric patients.
August 2021 marks the fourth year since the U.S. Food and Drug Administration approved cellular therapy implementing specialized chimeric antigen receptor T-cells for cancer treatment.
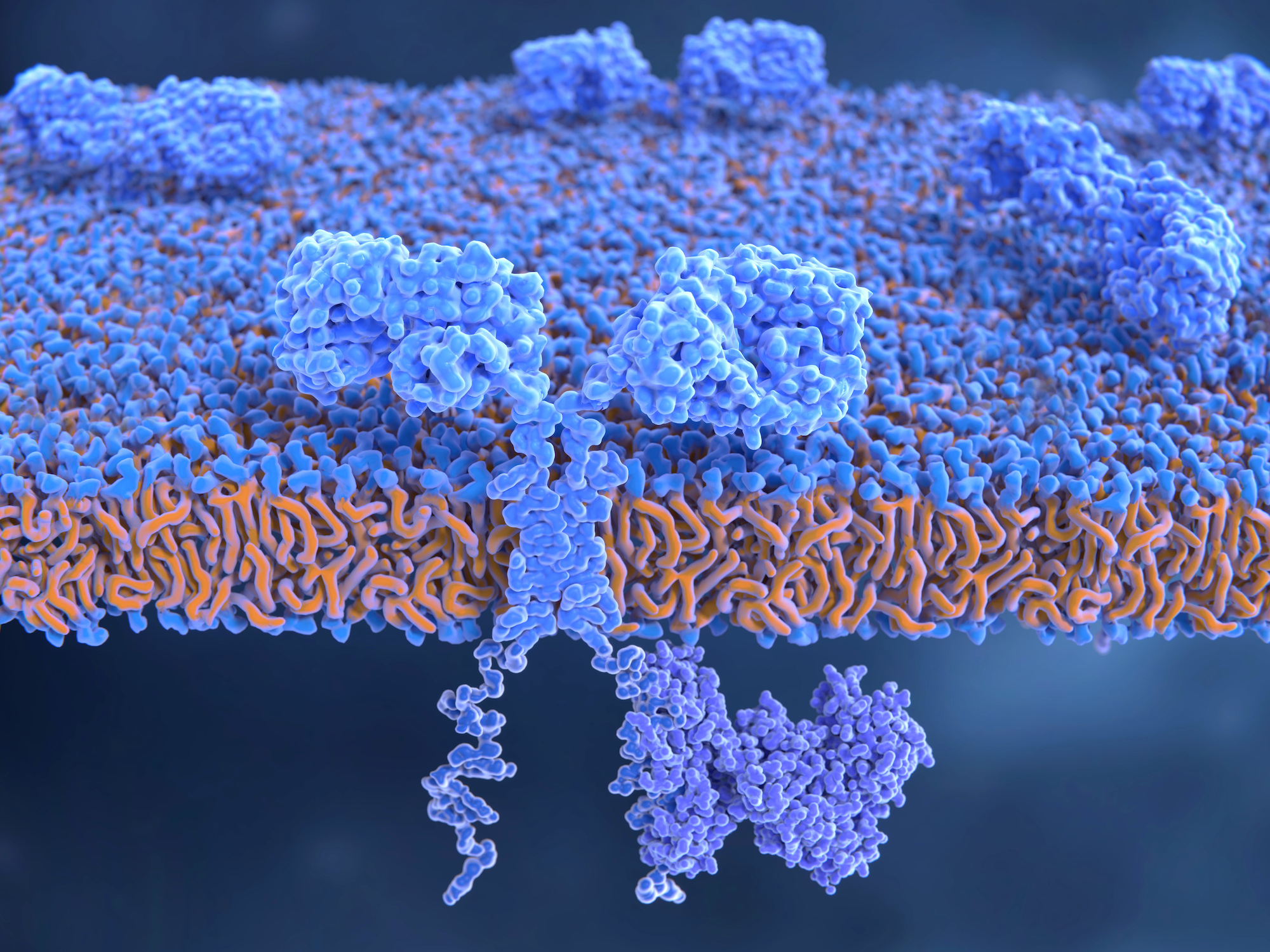
These CAR T-cells (as they’re known colloquially) form a type of protein with genetically-modified T-cells that are engineered to replicate an artificial T-cell receptor used clinically within immunotherapy. Unlike pre-existing, naturally-formed T-cells, these CAR T-cells are able to target certain proteins, specifically cancerous cells invading the body.
In efforts to improve cancer immunotherapy and commercialize the treatment introduced by CAR T-cells, the University of Pennsylvania alongside the Children’s Hospital of Philadelphia established Kymriah™ with Novartis and the Lymphoma Research Foundation for the CAR T-cell therapy.
Specifically, research and clinical trials at Penn’s Perelman School of Medicine and CHOP worked in collaboration with facilities from Novartis to gain FDA approval.
This breakthrough was especially positive for young patients who sought treatment for various forms of blood cancer. With CAR T-cells, patients could battle the cancer from within.
The new treatment would alter patients’ own T-cells within the immune system.
Then, at a Novartis manufacturing facility, the cells would be collected and modified to create CAR T-cells.
Finally, these potential CAR T-cells would distinguish cancerous cells from healthy ones, eventually destroying the invading leukemia cells. The specific protein they target in leukemia patients is known as CD19.
The CAR T-cells also act similarly to any immune system cells inside the body, and multiply at rapid rates — with even 10,000 new cells originating from one new CAR T-cell.
As a result of the successful cell engineering, leukemia patients have experienced high remission rates.
Initially, the treatment was created for patients suffering from B-cell precursor acute lymphoblastic leukemia (ALL) in refractory, second stages, or relapse.
In 2017, these patients could also be up to 25 years of age, but as the CAR T technology underwent numerous clinical trials, the ages of patients expanded.
At one trial at UPenn and CHOP implementing huCART19 in diagnosed B-ALL patients, the ages eligible for examination ranged from 1 to 29 years. However, the primary application of these CAR T-cells appeared to be within pediatric care.
RELATED CONTENT
The first pediatric patient in the world, six-year-old Emily Whitehead, was able to have treatment injecting the engineered CAR T-cells after searching for alternative care options for her leukemia.
Following close examination, Whitehead’s cancer appeared to be in remission, similar to the outcomes found in larger clinical trials.
Penn’s Abramson Cancer Center reported that after four years of FDA approval and five years after the initial treatment of Kymriah™ and CAR T-cells, non-Hodgkin lymphoma patients continue on their paths of remission.
Senior author Stephen J. Schuster, MD, the director of the Lymphoma Program at the Abramson Cancer Center, and assistant professor in Hematology-Oncology at the Perelman School of Medicine Marco Ruella, MD worked in CAR T-cell research to discover the outcomes of this FDA-approved cellular therapy.
According to Penn Medicine’s news journal, after examining 24 patients with an aggressive form of lymphoma who had treatment after their cancers, came back following standard care
“Forty-six percent achieved complete remission and 31% achieved progression-free survival at five years,” read the Penn Medicine report.
Also, following a separate 14 patients with another form of non-Hodgkin’s lymphoma, “71% achieved complete remission and 43% achieved progression-free survival at five years.”
This specific research underscores the most extended follow-up care relating to CAR T-cell therapy.
With official published data and an FDA approval, this form of immunotherapy is proving to be effective within both pediatric and adult patients with relapsed or refractory large B-cell (aggressive) lymphomas.










LEAVE A COMMENT: